You are only seeing posts authors requested be public.
Register and Login to participate in discussions with colleagues.
Medical Journal News
[Department of Error] Department of Error
[Articles] Appendicectomy versus antibiotics for acute uncomplicated appendicitis in children: an open-label, international, multicentre, randomised, non-inferiority trial
[Clinical Picture] Acute traumatic diaphragmatic hernia in a 4-year-old boy in collision with a speeding motorcycle as he crossed the road
[Seminar] Acute kidney injury
[Review] Multidrug-resistant Gram-negative bacterial infections
[Wakley-Wu Lien Teh Prize Essay] 破茧
UK covid inquiry: Bereaved families question vaccination strategies
US task force recommends osteoporosis screening to prevent fractures in older women
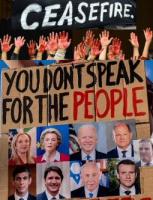
Gaza: Aid agencies ready to enter territory if ceasefire holds, but $10bn is needed to rebuild health system
Roll out and prospects of the malaria vaccine R21/Matrix-M
by Lorenz von Seidlein
In this Perspective article, Lorenz von Seidlein outlines the promise of two malaria vaccines, and discusses some of the considerations for their roll out.Effect of nirmatrelvir/ritonavir (Paxlovid) on hospitalization among adults with COVID-19: An electronic health record-based target trial emulation from N3C
by Abhishek Bhatia, Alexander J. Preiss, Xuya Xiao, M. Daniel Brannock, G. Caleb Alexander, Robert F. Chew, Hannah Davis, Megan Fitzgerald, Elaine Hill, Elizabeth P. Kelly, Hemalkumar B. Mehta, Charisse Madlock-Brown, Kenneth J. Wilkins, Christopher G. Chute, Melissa Haendel, Richard Moffitt, Emily R. Pfaff, the N3C Consortium
BackgroundNirmatrelvir with ritonavir (Paxlovid) is indicated for patients with Coronavirus Disease 2019 (COVID-19) who are at risk for progression to severe disease due to the presence of one or more risk factors. Millions of treatment courses have been prescribed in the United States alone. Paxlovid was highly effective at preventing hospitalization and death in clinical trials. Several studies have found a protective association in real-world data, but they variously used less recent study periods, correlational methods, and small, local cohorts. Their estimates also varied widely. The real-world effectiveness of Paxlovid remains uncertain, and it is unknown whether its effect is homogeneous across demographic strata. This study leverages electronic health record data in the National COVID Cohort Collaborative’s (N3C) repository to investigate disparities in Paxlovid treatment and to emulate a target trial assessing its effectiveness in reducing severe COVID-19 outcomes.
Methods and findingsThis target trial emulation used a cohort of 703,647 patients with COVID-19 seen at 34 clinical sites across the United States between April 1, 2022 and August 28, 2023. Treatment was defined as receipt of a Paxlovid prescription within 5 days of the patient’s COVID-19 index date (positive test or diagnosis). To emulate randomization, we used the clone-censor-weight technique with inverse probability of censoring weights to balance a set of covariates including sex, age, race and ethnicity, comorbidities, community well-being index (CWBI), prior healthcare utilization, month of COVID-19 index, and site of care provision. The primary outcome was hospitalization; death was a secondary outcome. We estimated that Paxlovid reduced the risk of hospitalization by 39% (95% confidence interval (CI) [36%, 41%]; p < 0.001), with an absolute risk reduction of 0.9 percentage points (95% CI [0.9, 1.0]; p < 0.001), and reduced the risk of death by 61% (95% CI [55%, 67%]; p < 0.001), with an absolute risk reduction of 0.2 percentage points (95% CI [0.1, 0.2]; p < 0.001). We also conducted stratified analyses by vaccination status and age group. Absolute risk reduction for hospitalization was similar among patients that were vaccinated and unvaccinate, but was much greater among patients aged 65+ years than among younger patients. We observed disparities in Paxlovid treatment, with lower rates among black and Hispanic or Latino patients, and within socially vulnerable communities. This study’s main limitation is that it estimates causal effects using observational data and could be biased by unmeasured confounding.
ConclusionsIn this study of Paxlovid’s real-world effectiveness, we observed that Paxlovid is effective at preventing hospitalization and death, including among vaccinated patients, and particularly among older patients. This remains true in the era of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Omicron subvariants. However, disparities in Paxlovid treatment rates imply that the benefit of Paxlovid’s effectiveness is not equitably distributed.